|
|
| The hepatitis B virus impact |
| By Jim Montalto, News Editor |
| Published: 09/07/2006 |
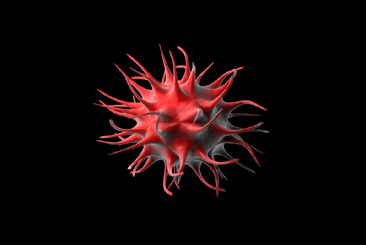 The Infectious Diseases in Corrections Report recently released its August issue on managing hepatitis B virus infection in response to the challenge viral hepatitis continues to pose to correctional populations. Research collected by IDCR suggests that more than 40 percent of inmates in some systems are infected with hepatitis C virus (HCV). Meanwhile, hepatitis B virus (HBV) outbreaks are also now being reported by facilities. This is complicating correctional health management because these viruses can co-infect HIV-positive individuals and increase mortality rates.
The Infectious Diseases in Corrections Report recently released its August issue on managing hepatitis B virus infection in response to the challenge viral hepatitis continues to pose to correctional populations. Research collected by IDCR suggests that more than 40 percent of inmates in some systems are infected with hepatitis C virus (HCV). Meanwhile, hepatitis B virus (HBV) outbreaks are also now being reported by facilities. This is complicating correctional health management because these viruses can co-infect HIV-positive individuals and increase mortality rates. Dr. David Alain Wohl, IDCR editor and Associate Professor of Medicine with the AIDS clinical trials unit at the University of North Carolina in Chapel Hill says, “Recent data describe increasing rates of mortality due to viral hepatitis among HIV-infected persons and liver disease is becoming a leading cause of death among patients with HIV. Given the heavy burden of hepatitis in prisons and jails, correctional clinicians must become familiar with the detection, prevention and management of both HCV and HBV.” Instead of writing an extensive analysis on this issue, IDCR changed tactics this month by interviewing Dr. Chloe Thio, a nationally recognized expert on HBV therapeutics and an associate professor of medicine at Johns Hopkins Medical School. Thio specializes in patients with HIV and viral hepatitis co-infection and conducts clinical investigations of HBV therapy. She recently published an article in Clinical Infectious Diseases titled, "Treatment of Chronic Hepatitis B Infection in HIV-Infected Persons: Thinking Outside the Black Box." Wohl's questions are pointed and cover a range of ideas from managing active HBV in inmates who are also HIV positive and have a high CD4 cell count, to the need for liver biopsies to help practitioners decide how to best treat HBV. "Dr. David Wohl (DW): The prevalence of hepatitis B virus (HBV) in prisons and jails in the US is several fold higher than the general population, and in many correctional facilities HBV screening is routinely conducted in inmates who are HIV-infected, therefore, I want to start by asking you about the management of HBV in the HIV-infected patient. What is your approach to managing HBV in HIV+ inmates who have active HBV but also have a high CD4 cell count and no indication for HIV therapy? Dr. Chloe Thio (CT): Before I would even consider HBV therapy in a newly diagnosed patient with active HBV infection, I would monitor them for six months to a year just to be sure this is a chronic infection and not acute HBV. Specifically, I would look to see if hepatitis B surface antigen (HBsAg) was lost or if the serologic pattern shifted from hepatitis B e antigen (HBeAg) positive to negative. This would help me determine if this was a person in the midst of a recent infection and possibly clearing their virus. Importantly, even if this is chronic HBV infection, a small proportion of people will clear the virus on their own - approximately 0.5% per year (1). So, I would monitor closely for a time, as I'd want to be sure I know the patient before starting therapy, especially since HBV therapy is not as effective as we would like. However, if the patient has evidence of end-stage liver disease I would consider therapy sooner." Wohl continues with specific therapies and when to apply them. "DW: If you were going to start HIV therapy what would you choose? CT: I use tenofovir (Viread) along with lamivudine or emtricitabine (Emtriva, FTC) - Truvada (Tenofovir+FTC fixed dose combination) is easy to use. Obviously, in a patient with lamivudine-resistant HBV, emtricitiabine would not be an active drug but we have learned from the HBV mono-infected that in lamivudine-resistant patients treated with adefovir, co-administration of lamivudine delayed adefovir resistance. So, I would use lamivudine or emtricitabine here even though there are no data looking at this phenomenon with tenofovir - but I am extrapolating from the adefovir experience. DW: What about HBV treatment for the HIV-uninfected patient? CT: What therapy I use depends on whether someone is HBeAg positive or not. If someone is HBeAg positive there is much more resistance data for entecavir than for tenofovir so if I am only going to use one, I would choose entecavir over tenofovir. Their potency is probably equivalent and my guess is that there will be little tenofovir resistance in the first year but it has not yet been studied in mono-infected patients so I tend not to use tenfovir alone and instead use Truvada - even in the mono-infected patients. Being HBeAg negative changes things and these are almost two different diseases. People with negative HBeAg require long-term therapy. Those who are HbeAg positive you are able to monitor for conversion to anti-HBe positive and then, when that happens, stop therapy six months after seroconversion occurs. In HbeAg negative patients if you stop therapy they almost always rebound. So, in the HbeAg negative situation I virtually never use mono-therapy since I know they are going to be on the drug a long time." Wohl asks comprehensive questions through out the discussion and Thio's answers are just as detailed, which is why we recommend reading the entire report at the IDCR website. An HCV case study highlighting major issues related to counseling, staging and treatment is also provided. |
MARKETPLACE search vendors | advanced search

IN CASE YOU MISSED IT
|


Comments:
No comments have been posted for this article.
Login to let us know what you think